Publish date: 15 August 2024
Artificial intelligence tech set to stay as it proves its worth in the fight against bowel cancer
Technology which uses artificial intelligence (AI) to spot abnormalities which may lead to bowel cancer is set to stay after a research study showed its value.
South Tyneside and Sunderland NHS Foundation Trust and Newcastle University led the COLO-DETECT trial. Northumbria Healthcare was among the trusts which took part in the trial.
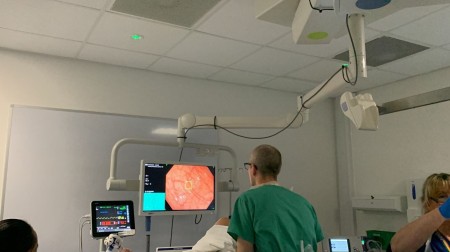
The trial used the GI Genius™ AI device, a computer module powered by AI which is added to the existing technology used during a colonoscopy. Colonoscopy is a procedure where a camera is used to look inside the bowel, with the aim of spotting cancerous and precancerous polyps (called adenomas).
GI Genius™ puts a green box around possible polyps on the screen which shows what the camera can see. The clinician then decides whether to remove the polyp.
The types of polyps which may turn into cancer are called adenomas.
COLO-DETECT was a randomised controlled trial where half of the participants had colonoscopy using AI and half had ‘traditional’ colonoscopy. It involved a total of 2,032 patients from 10 centres across England.
Using the AI during a colonoscopy showed it improves the detection of adenomas.
When using AI the study found:
- Using GI Genius found an extra 0.36 adenomas during each colonoscopy. This is a big difference when compared to other methods which have been used to try to improve the detection rate.
- Using GI Genius identified at least one adenoma in an extra 8 out of every 100 people having a colonoscopy.
- Using GI genius found increased detection of particularly worrying polyps called sessile serrated adenomas.
The findings of this research were published in Lancet Gastroenterology and Hepatology on Thursday, 14 August.
COLO-DETECT is part of COLO-SPEED, which is run from the North East of England and is one of the largest bowel cancer research groups globally.
COLO-SPEED stands for Colorectal Cancer Screening Prevention Endoscopy and Early Diagnosis and is funded by The Sir Bobby Robson Foundation, part of Newcastle Hospitals Charity, and the Parabola Foundation.
Professor Colin Rees, who led the trial, is a consultant gastroenterologist at South Tyneside and Sunderland NHS Foundation Trust and Professor of Gastroenterology at Newcastle University. He is also President of the British Society of Gastroenterology.
He said: "We are delighted with the outcome of this trial. Simply put, it will save lives.
"The fact that we recruited 2,032 patients across the country is phenomenal. I want to thank each patient who participated in this trial, because without them, we could not have completed this vital work.
"There has also been a tremendous effort by all of the research teams involved and I want to express my gratitude for their support.”
Discussing the findings, Prof Rees said: "This trial has demonstrated that using artificial intelligence can significantly increase detection of the kind of abnormalities in the bowel that may progress to cancer. We are able to find these lesions, remove them and stop these lesions turning into cancer.
"Crucially, we know that some of the polyps that lead to cancer are small polyps or flat polyps. The AI helped us find more of these lesions, the ones which are more likely to be missed with the human eye.
"There are 43,000 new cases of bowel cancer in the UK each year and sadly about 16,000 people die each year.
"To me that’s a tragedy, because bowel cancer is a disease that people shouldn't be dying from.
"We have a really long window of time when these polyps develop into cancer, probably about 10 to 15 years from developing a point to them becoming cancer.
"We have that period to find these lesions and remove them and reduce the risk of people getting cancer.
"We now use this technology routinely in our practice and I really hope that it will be used more widely.
"The fantastic thing about using AI is that it learns. It is trained by looking at images. It uses the data to find the differences between the images.
"It’s adding to its knowledge all the time, so it’s only going to get better."
Other findings of the trial were that more smaller polyps and more flat polyps were found when the kit was used than when it was not.
Using the technology did not increase the risk of complications during the procedure.
The addition of the technology added on average just 90 seconds to each colonoscopy.
The other trusts which took part were:
- Kettering General Hospital NHS Foundation Trust
- Bolton NHS Foundation Trust
- North Tees and Hartlepool NHS Foundation Trust
- The Royal Wolverhampton NHS Trust
- South Tees Hospitals NHS Foundation Trust
- University Hospitals of Morecambe Bay NHS Foundation Trust
- Newcastle Hospitals NHS Foundation Trust
- Gloucestershire Hospitals NHS Foundation Trust
- University Hospitals Sussex NHS Foundation Trust
