Health Inequalities Programme Board Annual Reports
Case studies 2024/25
Enhanced pathway of care
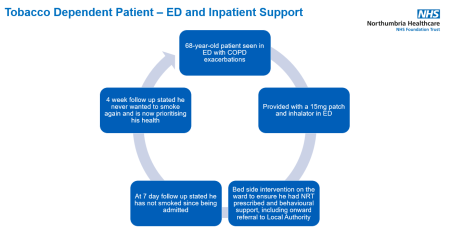
Inpatient support 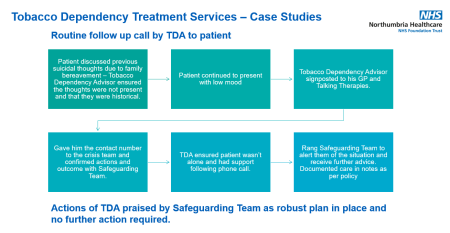
Case studies 2023/24
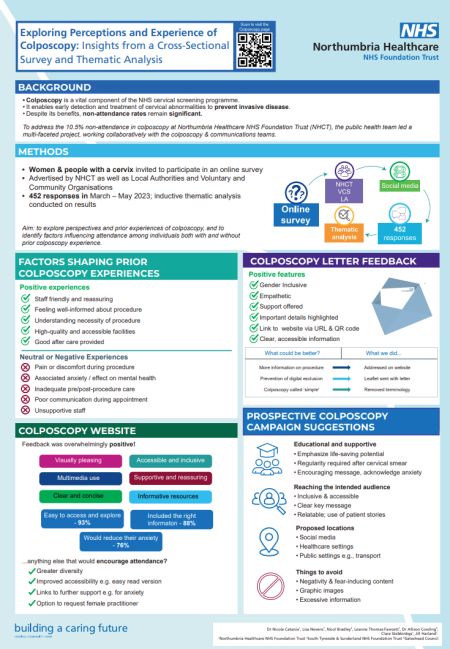
You can find out more about our colposcopy project here.
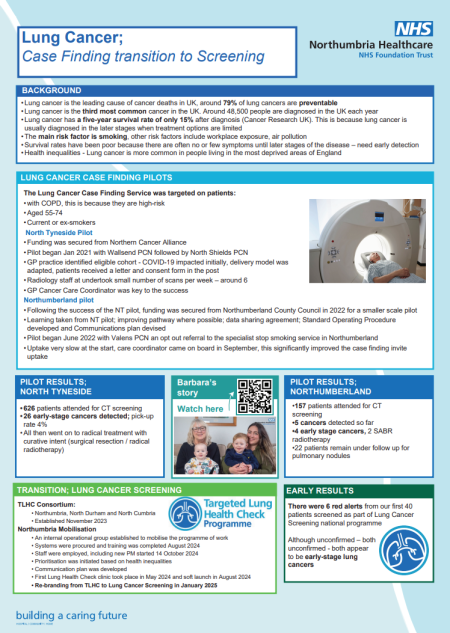
You can find out more about our lung cancer case finding pilot here.
In 2022, the UK National Screening Committee recommended introducing a targeted lung cancer screening programme across the UK. Following pilot schemes, it is now being rolled out across the country. The North project is a consortium involving Northumbria, North Cumbria, and County Durham and Darlington.
This has now launched with a roll-out taking place across Northumberland and North Tyneside from 2024 onwards.
Background
Smoking during pregnancy remains the single largest modifiable risk factor for adverse pregnancy outcomes, causing a significant risk to the unborn baby and a negative influence on maternal and child health, thus resulting in greater need for NHS and other statutory services.
Babies born to women who smoke have lower birth weights, are more likely to be born prematurely and are at increased risk of death within the first year of life. Most women who smoke in pregnancy are from areas of high deprivation and have correspondingly complex social needs and additional vulnerabilities.
Intervention
The project originated from NHS Long Term Plan direction to provide in-house smoking cessation support in maternity services. The work was led by the public health team with support and engagement from the trustwide maternity team. A key element to the introduction of the Best Start in Life team was listening to the patient's voice to ensure personalised care for those in need.
Key areas of focus:
- Flexible appointments including home visits.
- Local clinics: Advisors work in all Family Hubs; women are encouraged to register with the Family Hub and benefit from the range of services on offer.
- Non-judgemental approach – trusting relationship is vital.
- Support for partners and other family members offered.
The pathway supports the pregnant women from first ante-natal booking and identification of smoking status through pregnancy and postnatally (up to 2 contacts, day 1-5 and day 28).
Aims and objectives
Reduce smoking rates at delivery and the poor outcomes related to smoking in pregnancy. Provide holistic model of care to reduce health inequalities.
Key measures of success identified as:
- Better birth outcomes
- Smoking at Time of Delivery
- Quit rate
- Qualitative case studies
- Regional performance
Results
Smoking at time of delivery rates have shown a clear downward trend, with the latest quarterly figure (Q1 2024-5) of 5.8% for the trust sitting below the national ambition of 6%.
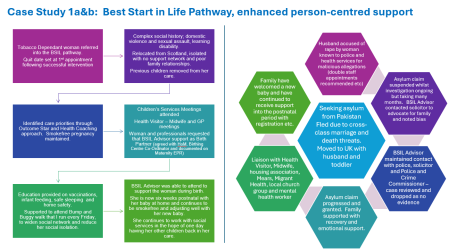
Background
As a trust, we did not adopt the enhanced continuity of care model, however, the public health team received funding to deliver the Best Start in Life (BSiL) enhanced continuity pathway. This workstream is currently supported by fixed term posts that have been extended to September 2025.
Intervention
The public health analytical team looked at bookings per year by Lower Layer Super Output area and then ordered them by deprivation – we then identified the areas which were most deprived and based on the bookings in those areas, chose the 4 most deprived which would allow the most effective caseload capacity.
This is also the area where the original continuity teams were based, the women here have the highest smoking in pregnancy rates, lowest breastfeeding rates and have more contacts with children's services, living with complex multiple vulnerabilities.
Based on the successful model of delivery for the BSiL smoking in pregnancy workstream, the enhanced continuity of care team offers:
- Opt-out referral based on postcode and/or ethnicity at booking.
- All women who are non-white British or Irish in Northumberland are referred into the service.
- 12 appointments including postnatal >28 days.
- Flexibility to avoid barriers to attendance - Appointments offered in homes, Family Hubs, cafes, leisure centres etc.
The team work to a holistic model of care, including:
- Healthy pregnancy support
- Emotional support
- Housing
- Finances and benefits
- Navigating systems – health/migration/local authority etc.
- Social isolation
Since November 2023, there have been 132 referrals (40 deprivation / 92 ethnic minority).106 women have accepted full support and are actively engaged with the service.
Treating tobacco dependency is one of the most cost-effective treatments we can offer patients. Many long-term illnesses and deaths are entirely avoidable by stopping smoking. An estimated 1 in 4 patients in acute hospital beds in England are smokers and around 60% of these want to stop smoking.
By consistently offering treatment and support to patients who use our services in Northumbria, we could prevent 480 deaths a year, reduce all cause readmission by 940 a year, save £1.5 million on readmissions and release 12 extra beds per day.
Intervention
The NHS Long Term Plan set a target by 2023/24, all people admitted to hospital who smoked would be offered NHS-funded tobacco treatment services. We have a dedicated inpatient Tobacco Dependency Treatment Service (TDTS) under the public health service. The TDTS has a number of key objectives including:
- To treat tobacco dependency as a long-term condition and ensure patients get treatment for their condition while in hospital.
- Identify patients who are tobacco dependant and provide treatment and behavioural support to enable a quit attempt.
To achieve this, the TDTS offer consists of:
Patient admitting team:
- Smoking status taken on admission (undertaken as part of nursing assessment)
- Provide nicotine replacement therapy (NRT) within 2 hours of admission – national reporting target.
- Add NRT to patient Emeds
- Provide 2 weeks supply on discharge.
TDA Team:
- Will identify patient from Nervecentre and visit patient within 24 hours to carry out full assessment (undertaken as an opt-out service)
- Provide behavioural support, promoting a quit attempt
- Refer for continued support into community provider provision
- Patient follow ups undertaken at week 1 and week 4 following discharge.
The public health team leads the Smokefree agenda and is working with a number of targeted teams to explore offering NRT at key contact points. Work is now embedded in surgical pre-assessment and in outpatients. All clinical teams can refer patients for support via ICE to community service provision; this offers best chance of a successful quit attempt.
Further work
The Smokefree lead and steering group are working to support further embedding of tobacco dependency treatment to allow patients to access timely NRT in their treatment pathway. Areas in scope include the emergency and urgent treatment departments.
You can found out more about our workforce health and wellbeing dashboard here.
Background
We offer Mini MOTs to staff at their workplaces during work time. They include a check of BMI; waist circumference; smoking status; blood pressure; heart rate; physical activity levels; musculoskeletal health; AUDIT-C score; WHO-5 Wellbeing Scale; sleep quality.
To support the NHS health check programme, the public gealth team liaised with occupational health to explore offering home blood pressure monitoring as part of the MOT offer to support case finding of hypertension among staff.
The Mini MOTs were targeted to our staff in lower bandings as we know from our staff Health Needs Assessment that they often have poorer health outcomes and are less likely to access staff support offers. During the period of delivering ad-hoc sessions, 298 mini MOTs were delivered between April 2022 and April 2023.
Aims:
- Upscale the mini MOT offer to provide 2-3 sessions per week over the pilot period.
- Support case finding of hypertension among staff by piloting home blood pressure monitoring (HBPM).
- Provide staff accessing a mini MOT with information to make informed decisions about their health to reduce risk factors.
Interventions
The following interventions were carried out over a 6-month pilot period (April 2023 to October 2023):
- Development and provision of a booklet to give to staff at mini MOT to record their measures and provide information on healthy ranges and where to access further information/support.
- Increased offer of mini MOTs and targeting of specific staff groups.
- Employ a member of staff on the bank to deliver MOTs.
- Offer self-referral to occupational health for HBPM to anyone that has high blood pressure at mini MOT who is not already on antihypertensive medication. Occupational health will then provide a letter to the staff member’s GP if hypertension is suspected.
Results and findings
265 Mini MOTs were carried out during the 6-month pilot period, compared to 104 in the previous 6 months. This was a 155% increase in the number of mini MOTs carried out during the 6-month pilot, compared to in the previous 6 months. If the additional bank staff member had been able to work to agreed capacity, a potential 468 Mini MOTs could have been carried out during the 6-month pilot period, however, 2 members of staff were recruited, but both went off sick after a few weeks in post which significantly reduced the offer.
69 people were found to have high BP at mini MOT. 56 of these were signposted to occupational health for HBPM. Eight of these self-referred to occupational health for HBPM. One person did not arrange to have HBPM. One staff member completed one week of home BP monitoring and was found to have a normal average BP, so no further action was needed. Six people completed HBPM and are undergoing further investigations and monitoring from their GP for a potential hypertension diagnosis. One staff member was directed to GP immediately due to significantly high reading and is now prescribed hypertension medication.
Recommendations
Provide additional permanent resource to continue delivering mini MOTs - link with provision of vaccinations and employ permanent member of staff to deliver MOTs for 6 months when not completing vaccinations.
Provide additional permanent resource to continue provision of HBPM as standard offer within the mini MOT.
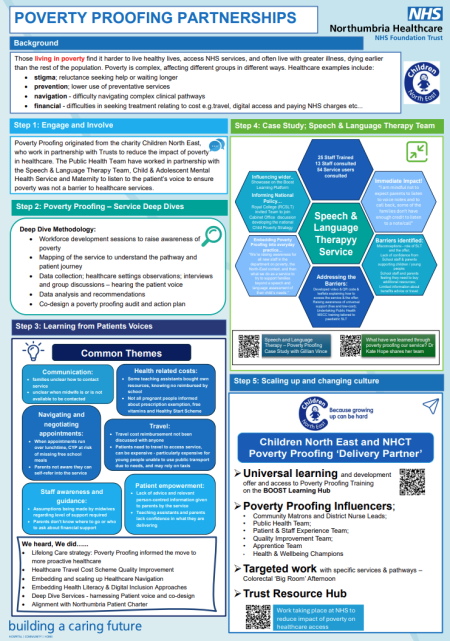
We are working in partnership with Children North East (CNE) on a collaborative process across targeted services. This process allows our services to identify and break down barriers for children and young people and their carers to accessing healthcare services.
In the North East, 38% of young people live below the poverty line. Studies have attempted to estimate the contribution of the wider determinants to population health; wider determinants have a greater influence on health than health care behaviour or genetics. The 10-year Marmot review and the Dame Carol Black review highlighted the huge economic costs of failing to act on the wider determinants of health.
It is recognised that healthcare access is a complex pathway for patients to navigate and poorly designed services in locations with access challenges can widen inequalities and increase poverty. Poverty proofing of our services can support services to minimise the impact of poverty on healthcare provision by reducing the impact of financial background on patient outcomes.
Well-designed services and pathways can increase uptake of early intervention services, reduce the financial burden of healthcare on low-income households and demonstrate a commitment to inclusive, accessible services.
The poverty proofing work is based on 3 principles:
- Poverty is a consequence of structural inequality, a need to address barriers by addressing policies, practices, systems, and structures to alleviate inequalities.
- Poverty impacts places differently, a need for robust understanding of the context of the local community.
- The voice of those with lived experience of poverty is the cornerstone of Poverty Proofing interventions.
The public health team has worked closely with targeted services to poverty proof key services supporting children and young people's opportunities to have the best start in life.
Actions are now being undertaken in the Speech and Language team (SaLT) and the Child and Mental Health Service team (CAMHS) are in the process of concluding their poverty proofing programme of work.
Next steps
In partnership with CNE and North East and North Cumbria ICB, our maternity services have commenced the poverty proofing process as part of the ICB exemplar pathways. This work is expected to conclude in May 2025.
Background
In the UK, Sudden Unexpected Death in Infancy (SUDI) is clustered in priority families (those with multiple vulnerabilities) for whom universal infant sleep safety guidance is not effective. Recent reports have highlighted the need for multi-agency working approaches. This project aimed to implement and evaluate a multi-agency SUDI prevention programme in Northumberland, one of England’s largest and most rural counties.
Methods
A steering group was identified to oversee the project representing a broad range of staff groups whose work brought them into contact with priority families in different ways in Northumberland.
The group decided which members of the multi-agency workforce should be invited to take part in the project. Job roles were grouped into 3 strands based on the frequency and type of contact with priority families.
Training was delivered via an online learning platform provided by the Durham Infancy & Sleep Centre team. Theory was used to support user engagement and embed SUDI prevention into everyday practice. Pre-and post-training surveys assessed staff knowledge and confidence with SUDI prevention, and follow-up surveys captured staff feedback and engagement.
Outcomes
Staff in 187 roles across 25 services were invited to take part and 1,007 staff registered for training. Eyes on the Baby training increased SUDI prevention knowledge and confidence across all strands; knowledge remained high two months after completion.
Staff commitment to SUDI prevention was sustained over time, however, some Strand 1 staff were initially dubious about their role in SUDI prevention, while others expressed strong enthusiasm. SUDI Champions played an active role in embedding SUDI prevention into everyday practice and Family Hubs were extremely active in parent engagement.
Health professionals were strongly in favour of the multi-agency approach to SUDI prevention and partnership working on SUDI prevention in priority families with colleagues across services.
Next Steps
Eyes on the Baby will be made available via the Northumberland Learning Together training platform to ensure SUDI prevention training continues to spread across the workforce.
Feedback from families is now needed to assess what information is reaching them, and via which channels.
Eyes on the Baby will be rolled out to other local authorities and services regionally, then nationally with a centralised oversight plan for governance and quality assurance.
Our public health matron is part of a national steering group which is working this up for NIHR funding to allow a national roll-out.
Background
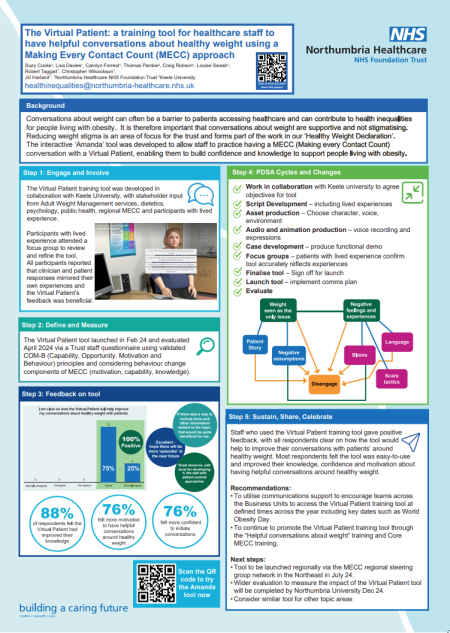
Our MECC vision is to develop our workforce to increase our approach on prevention, upskill staff with knowledge, resources and confidence to initiate lifestyle conversations, provide or signpost to interventions and ultimately improve physical and mental wellbeing and reduce the health inequality gap.
Our main priority is to expand the number of staff trained in MECC to embed the approach across the Trust. This aligns to the regional MECC strategy.
Our strategy committed to roll out MECC training at scale by building a network of ‘Train the Trainers’ (TtTs) who can then cascade the Core MECC training within teams and embed MECC within daily conversations. The training content has been adapted specifically for our audience to ensure that the 5-core health-related areas of MECC are given specific focus with a local overview of how to support and signpost patients in this regard.
Aim
Influence the culture of the organisation to one of proactive prevention with staff using MECC approaches wherever possible. An essential part of this is in supporting staff to feel confident and able to do this within their roles. This has meant creating a post-training offer of peer support meetings, additional training opportunities, engagement with the Regional MECC team and the development of a MECC portal within the trust.
Because of the size and complexity of the organisation, MECC training has been embedded within existing training and education programmes such as preceptorship, Care Certificate and Health and Wellbeing Champions training. This has allowed for a wide and consistent reach for the training programme.
Implementation
The vision for the MECC programme is two-fold. Firstly, it is to develop knowledge, awareness and confidence in the MECC approach via a training programme and building capacity within the organisation of staff who have this competency and secondly the aim is to ensure that we can evidence the embedding of MECC within patient pathways and services and be able to demonstrate that MECC conversations have taken place and advice/signposting provided as a result. This approach is being referred to as a gold standard MECC approach which includes the delivery of training for the service alongside provision of resources and support as well as moves to include MECC discussions in clinical notes.
Results and findings
Overall, 713 members of staff were Core MECC trained in Phase 1; 283 members of staff self-signed up and attended Core MECC, and 430 attended through embedded pathways.
Recommendations
- MECC to be included as part of annual plans for 2024/25. Include specific SMART objectives and an annual target.
- Targeted approach to embedding MECC within trust settings that have senior manager buy-in and support.
- MECC questions to be included in clinical systems
- Create a standardised way of recording and monitoring MECC training in the trust.
Overview
We have adopted the NHS Healthy Weight Declaration (HWD) as part of our strategic, system-wide approach to promote healthier weight, good overall health and wellbeing and reduce health inequalities for the benefit of staff, patients and the wider community. We adopted our NHS Healthy Weight Declaration jointly with North Tyneside Council and Northumberland County Council in November 2022 and were the first trust to adopt the declaration post-pilot.
We have taken a staged approach to adoption and implementation of the declaration, which has involved the following key milestones:
- Gain senior leadership buy-in
- Develop steering/planning group with key stakeholders
- Complete the HWD bench marking toolkit to ascertain current position, opportunities and gaps
- Develop Trust HWD action plan to set out our objectives against each commitment and timescales
- Develop comms plan
- Plan and deliver successful online joint launch with local authorities
- To work with local authority partners on a system wide approach across Northumberland and North Tyneside with a focus on staff and the patient population
- Monitor progress
- Evaluate impact of the plan
Implementation
The HWD consists of 16 commitments including food and drink provision, procurement, active travel, whole systems approach, supporting healthy weight in pregnancy, preventative approaches, MECC training, healthier vending, staff health and wellbeing. Our HWD action plan has detailed workstreams for each of the commitments.
One of the areas within the HWD we have progressed is weight stigma as we know this can be a barrier to accessing healthcare and can create health inequalities.
- We have developed a weight stigma environment and equipment checklist to ensure our environments and equipment are inclusive.
- We have developed ‘Helpful conversations about Weight’ training for our staff which launched in August 2023.
- We have worked in partnership with Keele University to develop an interactive virtual patient training tool to enable staff to practice conversations with the virtual patient. This launched in February 2024.

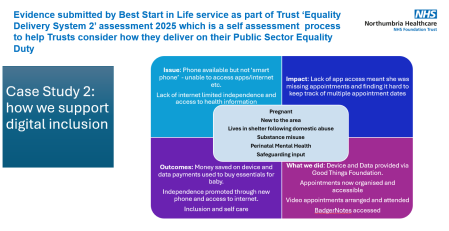
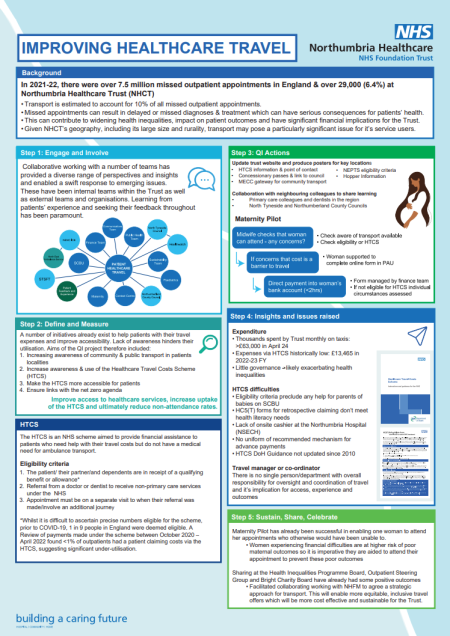
Background
In 2021-2022, there were over 7.5 million missed outpatient appointments in England. Transport issues have been estimated to account for approximately 10% of missed outpatient appointments. Transportation costs, complex or lengthy journeys and limited public transport options present significant barriers to patients accessing healthcare services. These challenges can lead to delayed or missed diagnoses and treatment and thus, can have serious consequences for patients’ health and contribute to widening health inequalities.
We serve one of the largest geographical areas of any NHS trust in England. Given more than 30% of scheduled outpatient appointments are for patients residing in rural locations, where there are often less accessible and reliable public transport options available, transport may pose a particularly significant issue for our patients.
Recognising the need to address transport as a barrier, a dedicated healthcare travel working group has been established.
Interventions
Several existing schemes and interventions aim to aid patients with travel costs or improve their journey accessibility. However, lack of awareness among patients often hinders take-up. As part of ongoing quality improvement efforts, enhancing patient awareness of these schemes is prioritised through improved patient communication. This includes disseminating information about concessionary passes for individuals over 65 or with specific disabilities, the North East Ambulance Service's eligibility criteria for non-emergency patient transport service, as well as local community transport options.
One such scheme, the Healthcare Travel Costs Scheme (HTCS), provides financial assistance to patients requiring help with their travel costs who do not have a medical need for ambulance transport. Eligibility criteria include receipt of qualifying benefits, referral by a doctor or dentist for non-primary care services under the NHS, and the appointment to which they are referred is on a separate visit to that in which the referral was made or requires an additional journey. Uptake of the HTCS by our patients has historically been very low.
By enhancing awareness and accessibility of the scheme among patients and staff, efforts aim to increase use of the scheme. This includes piloting a mechanism within maternity services to provide direct payments to patients for their transport costs in advance of their appointment. By facilitating attendance for patients who may have otherwise lacked the means, the overarching goal is to reduce non-attendance rates across the trust.
Background
Health coaching is part of the NHS Long Term Plan’s commitment to ensure personalised care, whereby people have choice and control over the planning and delivery of their care. Health coaching is based on what matters most to a patient and uses their own assets, strengths, and aspirations to improve health and wellbeing in the wider sense.
Health coaches work with patients with both physical and/or mental health conditions as well as those with long-term conditions or who may be at risk of developing them.
In May 2022, a new health coach model was developed in line with the NHSE Workforce Development Framework for health and wellbeing coaches. A pilot of a new model within specific clinical pathways took place from April to September 2023 to offer behaviour change advice and support as soon as possible within referral to pathways to support better health outcomes.
Aim
The new model was piloted in the following pathways:
- Public health maternity
- Colorectal cancer (Health While Waiting)
- Orthopaedics pre-assessment (Health While Waiting)
- Respiratory
- Physio – Movement in Medicine outpatient sessions
- Generic referral - all clinicians
Results and findings
The 6-month pilot highlighted that this is an effective role within secondary care and can support patients to make positive behaviour changes to improve health outcomes and support access to community-based services/assets. Patient feedback has been positive and health coach interactions have resulted in patients making positive behaviour changes.
Recommendations
- Remove generic health coach offer and non-clinical health coaching as this is provided in primary care.
- Focus on targeted and clinical health coaching (specific pathways or conditions). This would help define the role in secondary care and hopefully retain staff.
- Health coaches to be line managed and embedded as substantive members of staff within clinical team with professional support from public health to address barriers relating to feeling part of MDT and access to appropriate infrastructure.
- Health coaches to use same clinical system as clinical team rather than setting up specific health coach recording system.
- Health coach outcomes to align with clinical team outcomes to support any national targets.
- Health coaches to support prehab pilot from February to August 2024.
